Awe might seem an unobtainable luxury to many but, with the right approach, you can enjoy it daily – no mountain required.
On a crisp, clear day in January about four years ago, my children and I joined a few thousand Rhode Islanders in a protest march against a recent change in law that restricted the number of refugees who could enter the United States. As I held the hand of my four-year-old son, I was overcome with emotion. ‘No hate, no fear, refugees are welcome here,’ the crowd chanted as we marched through the streets, my six-year-old daughter joining in stone-faced. With a tightness in my chest and tears in my eyes, I could barely join along without choking up.
At the time, I didn’t have a word to describe exactly what it was that I was feeling, but now I do: awe.
Since the march, I had a spell working as a research and writing fellow at the Greater Good Science Center based at the University of California, Berkeley, which gave me the opportunity and privilege to delve into the burgeoning science of this emotion. The more I learned about it, the more I came to believe that it’s worth recognising awe and trying to cultivate it in our lives.
For centuries, mystics, religious scholars, philosophers and artists have had differing understandings of what the word ‘awe’ means. It originally connoted fear and dread toward divine beings, but now has a more general meaning encompassing a wide variety of experiences. ‘I define it as the feeling of being in the presence of something vast and mysterious that you don’t understand with your current knowledge,’ says Dacher Keltner, the founder and a faculty director of the Greater Good Science Center, and a leading researcher into the psychology of awe.
New York City Therapist Carolyn Ehrlich focuses on learning how we share space with each other. In therapy, both parties are given the opportunity to speak, guided by a therapist. And most importantly, both will be heard.
A landmark new scientific conceptualisation of awe by Keltner and his fellow psychologist Jonathan Haidt was published in 2003, based on what had been written about it from the fields of religion, philosophy, sociology and psychology. They proposed that, as varied as awe experiences can be, they all share two features: ‘perceived vastness’ and a ‘need for accommodation’.
According to this framework, while the perceived vastness of dramatic vistas such as canyons and mountains can provoke strong feelings of awe, this aspect of the emotion isn’t limited to literal size. Rather, it encompasses ‘anything that is experienced as being much larger than the self, or the self’s ordinary level of experience’, such as I felt on the Rhode Island march, but other related triggers might be extreme ‘social size’ (fame, prestige or authority), conceptual complexity and even outstanding moral goodness.
The other component of awe, ‘need for accommodation’, refers to the way the emotion forces us to change our understanding of the world. Awe can seem mind-bending in part because it is; it forces us to adjust our mental structures to assimilate new information (recent research scanning people’s brains while they experience awe suggests that this effect manifests at a neural level in decreased activity in the left middle temporal gyrus, a brain area that’s known to be involved Couples Therapy Tribeca in adjusting one’s previous schemas and understandings in light of new events and experiences).
Awe isn’t always experienced as a purely positive emotion. In around a quarter of awe experiences, people also report feeling a layer of fear. Imagine the mix of awe and alarm you might feel if you stumbled upon a grizzly bear on a hike, were stuck in a thunderstorm, or contemplated going to Hell. Early evidence suggests that this kind of threat-based awe might be more prominent outside the Western European and North American populations that have been the source of many awe studies. ‘You find more threat-based awe in hierarchical cultures,’ says Keltner. That said, his work has found that, at least in the Western world, most awe experiences are positive and have positive effects. ‘A quarter of the experiences are threat-based but three-quarters are really about exploration and connection, and have a lot of delight in them,’ says Keltner.
There’s a lot we can gain from those more delightful awe experiences. In the past nearly two decades of research on awe, dozens of studies have unearthed benefits associated with the emotion. ‘On all the major checkboxes of what’s good for you, it does a pretty good job,’ says Keltner.
For starters, there appears to be a connection between experiencing awe and better physical health. In a recent study, Jennifer Stellar, a psychologist at the University of Toronto, found that awe was one of the positive emotions most strongly associated with having lower levels of proinflammatory cytokines – protective proteins that are released when you get injured or ill, but which can have negative effects on health when they’re chronically elevated, including raising the risk of cardiovascular disease, diabetes and depression.
In terms of awe’s psychological benefits, there’s even more compelling evidence, with research linking greater experience of the emotion to more life satisfaction, increased humility, better mood, dampened feelings of materialism, and greater scepticism toward weak arguments.
Awe can make us better social beings, too. In multiple studies, participants who have been asked to write about an awe experience or who experienced awe in an experiment displayed more generous and cooperative behaviour than people who were induced to feel other emotions.
Besides boosting life satisfaction and making you a kinder person, awe experiences often just feel good – and important. ‘People report it being a very profound experience to have awe,’ says Stellar. ‘It also makes people see the world in a different way, and I think that’s valuable in its own right.’
Awe might feel profound in part because it encompasses a number of transcendent phenomena. It can change our perception of time, making it seem more plentiful and expansive, allowing us to savour the here and now. During awe, people also report feeling less significant and smaller relative to their environment – a positive effect that researchers term ‘the small self’.
‘When people feel shame, they feel very small, but they also feel very aware of themselves, which is different than awe where they feel small but not so aware of themselves,’ says Stellar. ‘[Awe] seems to be this very interesting situation where you can feel self-diminishment, but it’s a good and exhilarating feeling.’ At a neural level, brain imaging research suggests that this is reflected in reduced activity in the ‘default mode network’, a network of brain regions that are particularly active when our minds are wandering or we’re thinking about ourselves (similar neural effects are observed during meditation, states of flow and psychedelic trips).
While awe makes us less focused on ourselves, evidence suggests it also makes us feel more connected to other people, more a part of a greater whole and something larger than ourselves. In this way, it creates a bridge between what Keltner calls the ‘default self’ – our drive to do well, meet our goals, protect ourselves, rise in status – and our desire, and indeed need, to be part of society and help others. ‘I’ve got to protect myself, but I’ve got to serve the collective – that’s one of the great tensions in identity and in our evolution,’ says Keltner.
While we can imagine how, in the wrong hands, this bridge can be used as a force for manipulation – think of a charismatic cult leader or suicide bomber – the transformative effects of awe can also be powerfully positive. ‘[I]t seems to be this really important emotion for when we’re confronting things that might be scary and bigger than us and hard to understand, but it’s the positive side of that,’ says Stellar. ‘It’s so embedded into humanity’s goal of trying to understand the world better and really taking on that challenge and those scary, unfamiliar parts, rather than shying away from it.’
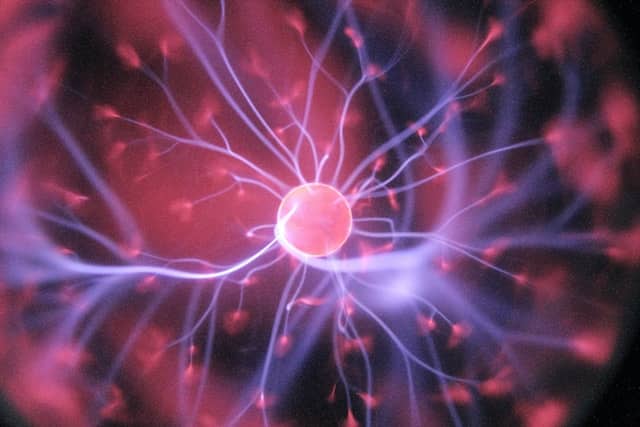
All that being said, some of us are clearly more awe-prone than others. Modern life can also make awe feel inaccessible. If your life is packed full of work stress, domestic demands and commercialised spaces, you might feel that experiencing awe in your day-to-day existence is a challenge – or even an unobtainable luxury. I know I’ve felt that way, especially in the middle of a global pandemic when I’ve rarely left my suburban home and found myself in a loop of repetitive routines. Fortunately, there’s research suggesting that we don’t need to step out of our everyday lives to experience more awe, and in this Guide I’m going to show you how.
What to do
To foster more awe in your life, Keltner recommends exploring the ‘eight wonders of life’. Before I share these wonders with you, here are a few broad considerations that might make it more likely that you’ll have an awe experience:
*If possible, limit distractions. Complete the task that has been nagging you. Turn off notifications on your phone (or leave it in another room or at home). Ask your partner, roommate and/or children for some space.
*Treat your awe experience like a contemplative exercise. Begin with some deep breathing, and pay attention to the sound and feeling of your breath as you inhale and exhale.
*Turn your attention outward and be open to inspiration. Notice what catches your mind. Do some of your senses seem heightened? Do you feel goosebumps? Do you feel more curious? Delighted?
*Don’t worry if you’re not feeling awe. Awe is different for everyone, and some days you might just not be feeling it.
The nice thing is, once you start thinking about awe, you might begin to notice all the places it shows up in your everyday life. In other words, you might naturally experience awe more often as you start to pay attention to it, similar to how people often feel more gratitude once they begin a gratitude journal. Of course, not all awe experiences will move you to tears or make you feel at one with the Universe. Just as with other emotions, awe comes in a range of intensities – from the gentle awe you might experience on a walk through the woods to the life-changing awe you might experience at the birth of your child.
Some places I believe I’ve experienced awe include concerts, sporting arenas, movie theatres, the Badlands National Park, the Pacific Coast, in my previous life as a neuroscientist, and as a parent. ‘In our studies around the world, people are feeling it two or three times a week,’ says Keltner. ‘I think you can get a little dose every day.’
Now to Keltner’s Eight Wonders of Life – eight ways to seek out more awe:
1. Witness other people’s moral beauty and courage
The first wonder of life, according to Keltner, is other people’s moral beauty and courage. It’s easy to become awestruck by stories of courageous people such as Harriet Tubman, Martin Luther King, Jr or Greta Thunberg. Similarly, Stellar notes that movements for social change, such as Black Lives Matter and March for Our Lives, can be awe-inspiring for people. Generally speaking, Keltner thinks that we tend to discount the extent to which other people are important for awe. ‘We often think of awe as spiritual or natural – and that’s part of it – but the bigger story is it’s about our fellow human beings… We find that 50 to 60 per cent of awe experiences are just like you’re blown away by other people,’ he says. People can also feel awe when observing someone with incredible skill or talent or unique abilities (think Michael Jordan or a contortionist).
2. Move in unison with others
From ceremonial dances to army marches to tapping your toes in rhythm with a friend, humans have a natural proclivity for synchronised movement. Several studies have found that people are more cooperative and generous after moving in unison with others, and that they feel more bonded to their movement partners. Moving together appears to help strengthen social ties and, says Keltner, it can also elicit awe. To test out this wonder, try participating in a form of shared movement such as dance, exercise, playing music, singing in a choir, cheering on a sports team or even walking with a friend.
3. Get out in nature
Importantly, you don’t need to visit the Grand Canyon or the Great Barrier Reef to get a dose of awe from nature. ‘It can just be a walk through a forest that’s near your house,’ says Stellar. To get more awe out of an everyday hike, Keltner recommends taking time to deepen your thinking about the experience. ‘Start to look for patterns in nature, take a moment to think about what’s vast,’ he says. You might consider making a habit of going for ‘awe walks’. In a recent study, Keltner and his colleagues found that older adults assigned to take weekly 15-minute awe walks reported greater increases in positive emotions and decreases in distress in their day-to-day lives than did those assigned to a control walk condition. The Greater Good Science Center offers step-by-step instructions for getting the most out of an awe walk, including how to breathe and shift your awareness to what’s around you.
4. Listen to or create music
Listening to a symphony, singing in a choir, or playing an instrument can produce feelings of awe. If you’ve ever had goosebumps or what people call ‘the chills’ while listening to a particularly moving song, you were likely also experiencing awe. While listening to any form of music has the potential to elicit awe, songs that are exceptionally beautiful or complex are more likely to produce the emotion. Making music with others – be it in a choir, band or orchestra – might also increase the likelihood of awe because those activities have the added benefit of involving synchronised movement.
5. Take in visual art or film
Visits to art galleries and museums (in person or online), public art and sculpture, and movies with stunning visual elements can all provoke awe. Stellar, who lives in Toronto, says she normally seeks out awe in the city by going to museums and galleries. Visuals that might be more likely to evoke awe are those that are very large – such as Michelangelo’s David or the Taj Mahal – or very detailed, intricate or complex, such as a fractal or an exceptionally lifelike painting. Even the most common elements can produce awe when presented in a unique way. In one study, viewers experienced awe when they watched a slow-motion video of drops of coloured water falling into a bowl of milk.
6. Seek out a spiritual or religious experience
For people of faith, religious gatherings, ritual and prayer can be profound sources of awe. Meditation, Stellar notes, can also inspire awe for some. Even recalling a past spiritual or religious experience can evoke feelings of awe. In a 2017 study, participants who wrote about spiritual experiences reported higher levels of awe and a greater sense of ‘a small self’ than did control participants who wrote about humorous experiences. Both religious and non-religious participants experienced these effects despite recalling different types of memories. Religious people recalled more religious events as well as life-and-death events, whereas non-religious people were more likely to recall experiences with nature, science, yoga or meditation. The message here is that the types of experiences that you personally deem spiritually meaningful are the ones most likely to result in awe.
7. Consider a big idea
‘It gets kind of metaphysical,’ says Keltner. ‘Big ideas give people awe – like Marxism, free markets, evolution.’ You might have already had an experience in school or while reading that filled you with awe. The process of wrapping your mind around a new concept is cognitive accommodation, a key competent of awe. So if you take the time to grapple with a new, big idea for you – say quantum physics – that could bring more awe into your life. Similarly, Keltner says poetry that at first glance can seem difficult to comprehend can evoke awe when the reader discovers what the poem is about.
Another related way to add more awe to your life is to deepen your contemplation and curiosity about the world by posing questions or puzzles to yourself – to turn everyday experiences into a way to think about big ideas. For example, Keltner recommends thinking about clouds and how they work – or waves, or rainbows. This is a way to transform simple wonder into awe and discovery. He points out that the obsessions René Descartes and Isaac Newton had with rainbows led them to figure out the physics of light.
I’ve found that parenting can be a fountain of inspiration for this type of awe, both because I experience awe secondhand when my children understand something for the first time, and because human development (such as witnessing children learn to talk, read and do mathematics) is awe-inspiring.
8. Witnessing life and death
For parents, the miracle of pregnancy or birth can create feelings of awe. Contemplating or witnessing death, too, is often tinged with awe, although confronting this aspect of awe can be psychologically difficult. While you might not want to go out of your way to cultivate these experiences in your personal life for the sake of awe, life and death are prominent themes in many memoirs, novels and other forms of art.
Hopefully, one thing that comes across from Keltner’s Eight Wonders of Life is that awe can be found in many corners of our everyday lives. ‘We talk about it as if it’s a once-in-a-lifetime thing, but in fact it’s everywhere,’ says Keltner. That said, research suggests that some people – whether by personality and/or life circumstance – are more naturally prone to experiencing awe. If you’ve tried some of these activities and haven’t experienced awe, don’t despair. Keep seeking out new experiences that interest and excite you. Who knows? You might just discover a ninth wonder.
‘My big advice is that some people aren’t that into music or nature or whatever, but everybody can find something that makes them feel awe,’ says Stellar. ‘Awe is an amazing emotion and there are so many different ways people can experience it. Find that thing that does it for you and keep doing that.’
A note about psychedelics
An elephant in this awe-filled room is psychedelic use. According to Keltner, there is some theorising that the psychedelic experience is essentially the experience of awe. In a 2018 article, Peter Hendricks, a clinical psychologist at the University of Alabama at Birmingham, lays out the case for how ‘mystical experiences elicited by classic psychedelics appear to exemplify awe’.
Indeed, people who use psychedelics report feeling a sense of connectedness with humanity and oneness with the Universe, as well as a changing awareness of the self. In the scientific study of psychedelics, this is known as ‘ego dissolution’, which could be conceptualised as an extreme example of the small-self phenomenon common in awe experiences. Intriguingly, Hendricks also proposes that awe might be the mechanism that underlies the positive effects caused by psychedelic-assisted psychotherapy. While I can’t personally attest to or vouch for or against psychedelic use, this branch of awe research will likely continue to develop as a growing number of municipalities in the US – and the entire state of Oregon – have decriminalised use of the hallucinogen psilocybin. If you’d like to explore further, a previous Psyche Guide covered the basics of how to have a safe psychedelic trip.
*Awe is a complex emotion that tends to arise when you’re in the presence of something vast that you don’t already understand. It heightens your sense of time, makes everyday concerns fall from view, shifts your perspective, and makes you feel more connected with the world and part of a greater whole.
*Awe is usually, but not always, perceived as positive, and experiencing it more often is associated with a range of physical and psychological benefits including reduced inflammation, greater life satisfaction and humility.
*The vastness that provokes awe doesn’t necessarily have to mean physical size. Any type of stimulus that goes beyond your ordinary experience of the world could qualify, including objects or concepts that are especially complex or people who are exceptionally famous, prestigious or morally good.
*Awe is more common than you might think. People experience awe on average 2.5 times a week. You don’t need to summit a mountain to experience awe. It can be found in your own backyard, in a book or on the internet.
*Adopting the right mindset can increase your chances of experiencing awe, including deepening your breathing and turning your attention outward.
*Look to Keltner’s Eight Wonders of Life for experiences that can make you feel awe: moral beauty and courage, moving with others, nature, music, visual art and film, spiritual and religious experiences, big ideas, life and death.
*Awe experiences are different for everyone. What elicits awe in one person might not have the same effect on you. It’s worth trying a variety of experiences.
Learn more
Our notions about awe – what the emotion is like and what experiences are likely to inspire it – have changed over time. Nowadays, awe has mostly positive connotations, particularly in the Western world, but this wasn’t always the case. Even today, the Merriam-Webster dictionary defines awe as: 1) ‘an emotion variously combining dread, veneration, and wonder that is inspired by authority or by the sacred or sublime’, and 2) ‘[archaic] a: dread, terror; b: the power to inspire dread’.
To chart the meaning of awe over the centuries, Stellar teamed up with a linguist in her university’s computer science department to analyse how the usage of the word ‘awe’ has changed over time in Google’s corpus of texts. ‘There is evidence that it has changed to become more positive,’ says Stellar. ‘It looks like the time period in which it’s changing has to do with transcendentalism and Romanticism as philosophical movements that prioritise beauty in nature and spirituality.’ In other words, rather than being tied to scary gods and fearful experiences, awe began to be tied to beauty in nature, art and music.
This change in the cultural meaning of awe might mirror the changing relationship between people and nature. The American environmental historian William Cronon articulates this change in his essay ‘The Trouble with Wilderness; or, Getting Back to the Wrong Nature’ (1995):
Go back 250 years in American and European history, and you do not find nearly so many people wandering around remote corners of the planet looking for what today we would call ‘the wilderness experience’.
Whereas people today seek solace and awe on mountains and in canyons, this would probably have seemed strange to people in the 18th century or earlier, at which time Cronon says we were much more likely to associate being in wilderness with ‘bewilderment’ or ‘terror’ (and thus closer to the historic darker notions of awe).
One need only look at the Bible, says Cronon, in which the wilderness was a place where people found themselves in ‘moral confusion and despair’ – where Moses wandered for 40 years, and Christ struggled with the Devil, and where Adam and Eve were ousted to from Eden. ‘Wilderness, in short, was a place to which one came only against one’s will, and always in fear and trembling,’ writes Cronon.
This began to change with the spread of Romanticism. The Romantics had the idea that it is in sublime landscapes that people are most likely to experience the sacred and, in Cronon’s words, ‘glimpse the face of God’. Cronon adds: ‘He [God] would most often be found in those vast, powerful landscapes where one could not help feeling insignificant and being reminded of one’s own mortality … God was in the mountaintop, in the chasm, in the waterfall, in the thundercloud, in the rainbow, in the sunset.’
It’s true that early Romantic writers found these kind of nature experiences terrifying. Consider a poem by William Wordsworth about his visit to the Alps where his encounter with the divine evoked a decidedly terror-tinged sense of awe, with ‘Winds thwarting winds bewildered and forlorn’. But a century later, there are signs of this fearful attitude changing. Here’s the Scottish-American naturalist John Muir in 1911 describing Yosemite’s North Dome:
No pain here, no dull empty hours, no fear of the past, no fear of the future. These blessed mountains are so compactly filled with God’s beauty, no petty personal hope or experience has room to be. Drinking this champagne water is pure pleasure, so is breathing the living air, and every movement of limbs is pleasure, while the body seems to feel beauty when exposed to it as it feels the campfire or sunshine, entering not by the eyes alone, but equally through all one’s flesh like radiant heat, making a passionate ecstatic pleasure glow not explainable.
It’s clear that Muir is describing an awe experience here, complete with a changing perspective of time and diminishment of the self, in tune with the contemporary psychological definition of the emotion. This broader cultural shift also meant that by the late 1800s people were beginning to seek out experiences in nature. Natural sites in the US, such as Niagara Falls, the Catskills, Yosemite and Yellowstone, started to become tourist destinations. Wilderness was no longer a place to avoid out of terror or temptation, but rather a place to seek out beauty, the sacred, wonder and awe.
‘The Romantic legacy means that wilderness is more a state of mind than a fact of nature, and the state of mind that today most defines wilderness is wonder,’ writes Cronon in his 1995 essay, although he could just as easily have defined it as awe, wonder’s more magnificent cousin. ‘The striking power of the wild is that wonder in the face of it requires no act of will, but forces itself upon us – as an expression of the nonhuman world experienced through the lens of our cultural history – as proof that ours is not the only presence in the Universe.’
Links & books
My 2018 white paper for the Greater Good Science Center delves into dozens of studies about the science of awe. It includes a discussion about how to define awe, who is most (and least) likely to experience awe, why a feeling such as awe might have evolved, what experiences tend to elicit awe, and what’s known about the physical and psychological effects of awe.
The psychologist and awe researcher Dacher Keltner recommends checking out the Greater Good Science Center’s series of step-by-step awe exercises and this guided awe walk meditation through Muir Woods in California that he did for Mindful.org.
Keltner also recommends Alan Cowen’s Mapping Emotion website. By exploring these maps, you can see what sounds, videos and facial expressions correspond to awe and other emotions. In particular, he recommends the ‘Emotional Experiences Evoked by Video’ map that shows which emotions were most commonly evoked by 2,185 different short video segments. A research study about these findings was published in the Proceedings of the National Academy of Sciences.
The psychologist and awe researcher Jennifer Stellar recommends watching clips from the BBC Earth channel on YouTube, attending virtual or in-person concerts by a symphony orchestra, or visiting a photography exhibit hosted by a museum.
The ultimate awe experience might come from seeing Earth from space. A 2016 paper by the psychologist David Yaden includes several quotes from astronauts discussing this experience, sometimes called the ‘overview effect’. While most of us will never be able to truly experience this first-hand, you can still get a dose of awe from viewing the International Space Station’s live feed of Earth. In a similar vein, I use Chrome’s Earth View from Google Earth browser extension, which displays an image from across the globe each time I open a new tab.
Yaden founded the Varieties Corpus, a website where people can share and learn about self-transcendent and awe-inspiring experiences.
Perhaps surprising to some, Couples Therapy Tribeca social media can be a great place to encounter strange moments of awe. Some recent awe-inspiring posts I’ve seen on Twitter include a giant xylophone in the woods of Japan that plays Bach and a video of the surface of Venus.
Books that touch on personal awe experiences include Mountains of the Mind: Adventures in Reaching the Summit (2004) by Robert Macfarlane, A Private History of Awe (2006) by Scott Russell Sanders, and How to Change Your Mind: What the New Science of Psychedelics Teaches Us About Consciousness, Dying, Addiction, Depression, and Transcendence (2018) by Michael Pollan.
Summer Allenis a freelance science writer and former neuroscientist. She served as a research and writing fellow for the Greater Good Science Center at the University of California, Berkeley. Her work has appeared in The Washington Post, Mindful magazine, and other outlets. She lives in Portland, Oregon.
Photo: Pexels




















































































 Breathwork is generally a safe technique without any adverse health effects. However, it is possible experience one or more of the following if a technique is done wrongly or there is an underlying health condition:
Breathwork is generally a safe technique without any adverse health effects. However, it is possible experience one or more of the following if a technique is done wrongly or there is an underlying health condition: Breathwork is effective in increasing your quality of life. However, the technique requires focus to get the best out of it. It also needs a quiet place where you’ll not be distracted by noise.
Breathwork is effective in increasing your quality of life. However, the technique requires focus to get the best out of it. It also needs a quiet place where you’ll not be distracted by noise.





















